"We're embracing the digital frontier."
Axel Baur
CEO of Amplify Health Asia
Make strategic provider decisions
Health insurers face rising medical costs and a growing need to 'bend the curve' on the increasing cost of healthcare
Amplify Health's Provider Management Solution helps insurer health teams to engage and contract with providers more effectively.
It combines actionable analytics with expert advisory services to help manage care variation and slow claims cost inflation, whilst ensuring provider quality and accessibility for their members.
Provider Management Insights Suite

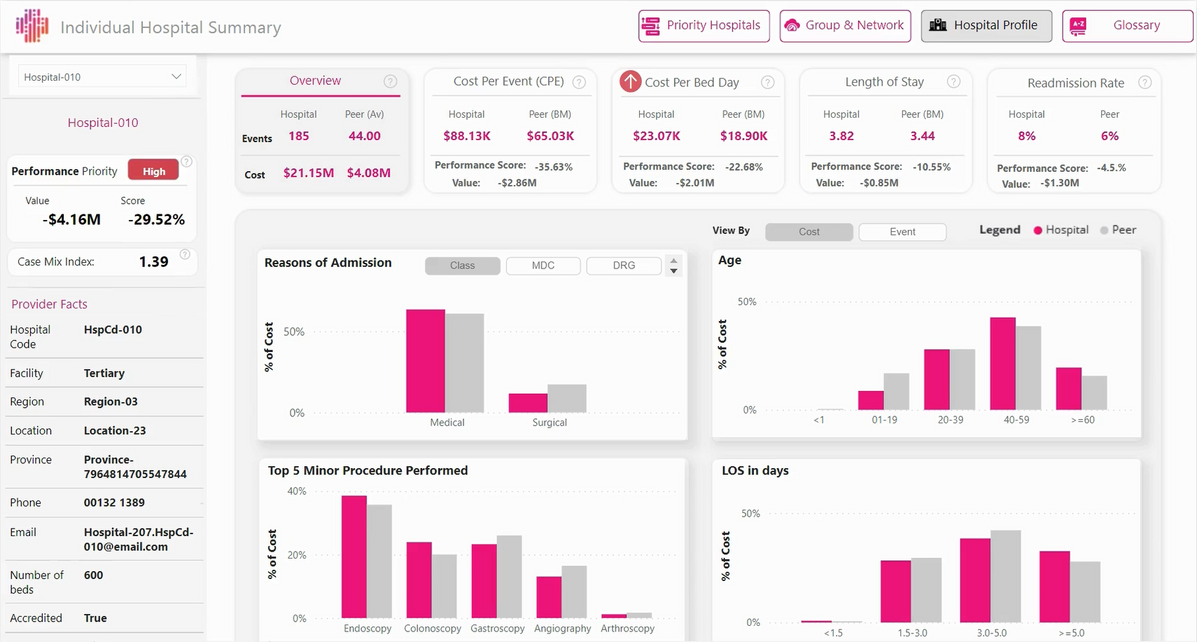
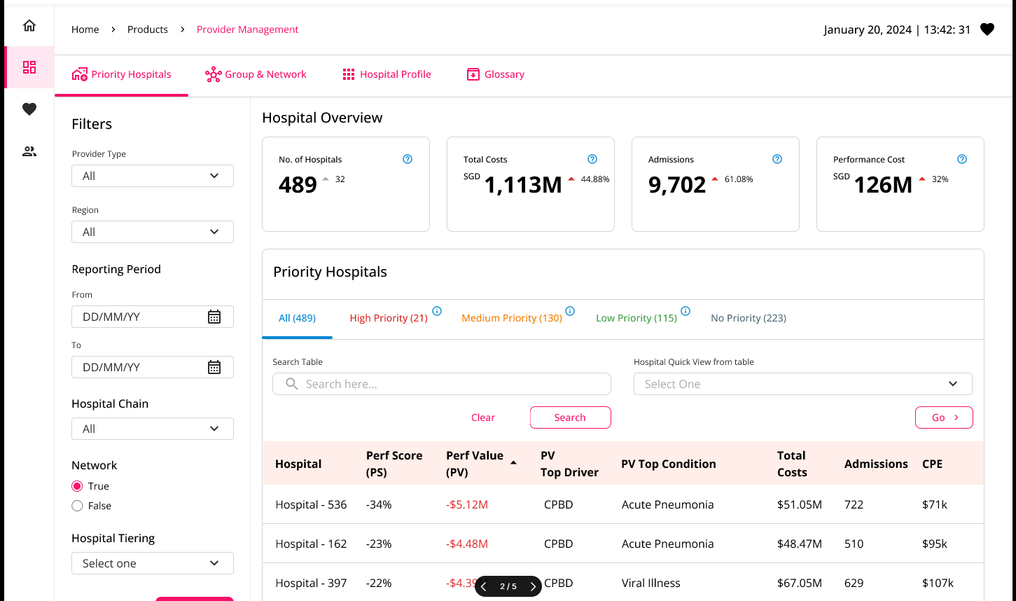
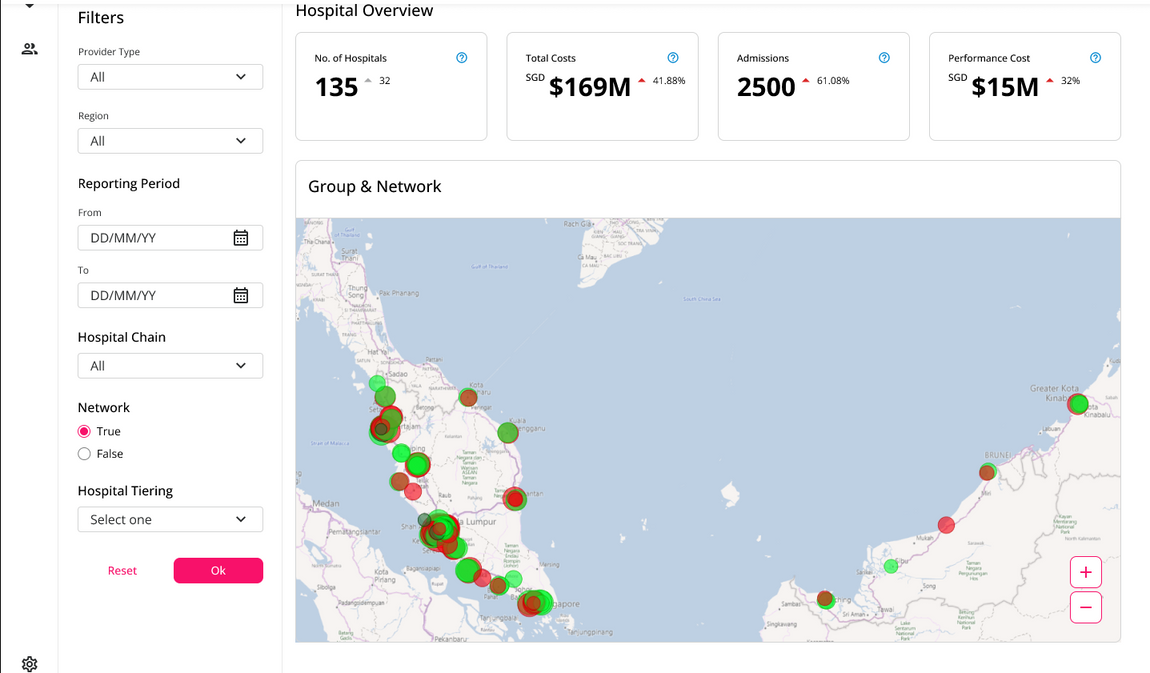
Hospital Network & Performance Profiles
Empower data-driven agreements with providers using validated performance benchmarks & efficiency opportunities.
Outpatient Network & Provider Profiles
Monitor & improve outpatient panel performance. Understand providers’ cost and referral patterns. Encourage patient-centric care with provider allocation metrics.
Bundled Pricing, Reference Fees Tool
Monitor existing bundled fee agreements for utilisation and savings. Design new bundled fees with clinical advisory and reference price data insights for fair, predictable agreements.
Hospital Network and Provider Profiles
Optimise inpatient networks and prioritise hospital engagements
Amplify Health’s analytics for hospital networks empower risk managers to actively monitor inpatient claims and contracted hospitals, based on overall performance across cost, utilisation and quality factors.
The risk-adjustment methodology combines both industry-standard Disease Related Grouper (DRG) algorithms, as well as trained machine learning models, to incorporate a wide range of risk factors at both the aggregate and per-event level.
Key Features & Reference Datasets
Hospital Profiles
The ‘Top Driver’ algorithm highlights greatest impact across Cost per Event, Length of Stay, Cost per Bed Day and more.
Inpatient Specialist Listings
Based on comparable medical or surgical practices, utilising common performance indicators.
Comprehensive Risk Adjustment Methodologies
Cater for patient case-mix complexities, differences between providers, as well as care settings.
Prioritise Top Conditions
Based reference data of over 1,100 diseases and procedures that contribute to the highest cost, over-utilisation etc.
Prioritise Provider Performance
Based on risk-adjusted benchmarks, historical trends and financial value of improving inefficiency.
Analyse Provider Groups
Meet network planning objectives, e.g. identify highly efficient providers for directing patients or establishing fee benchmarks.
Outpatient Network
and Doctor Profiles
Enjoy comprehensive and detailed information on patients and providers
For health insurance teams that manage both inpatient and outpatient providers, this module provides both an overall view of the outpatient network, GP and specialist panels, as well as individual doctor or practice performance profiles.
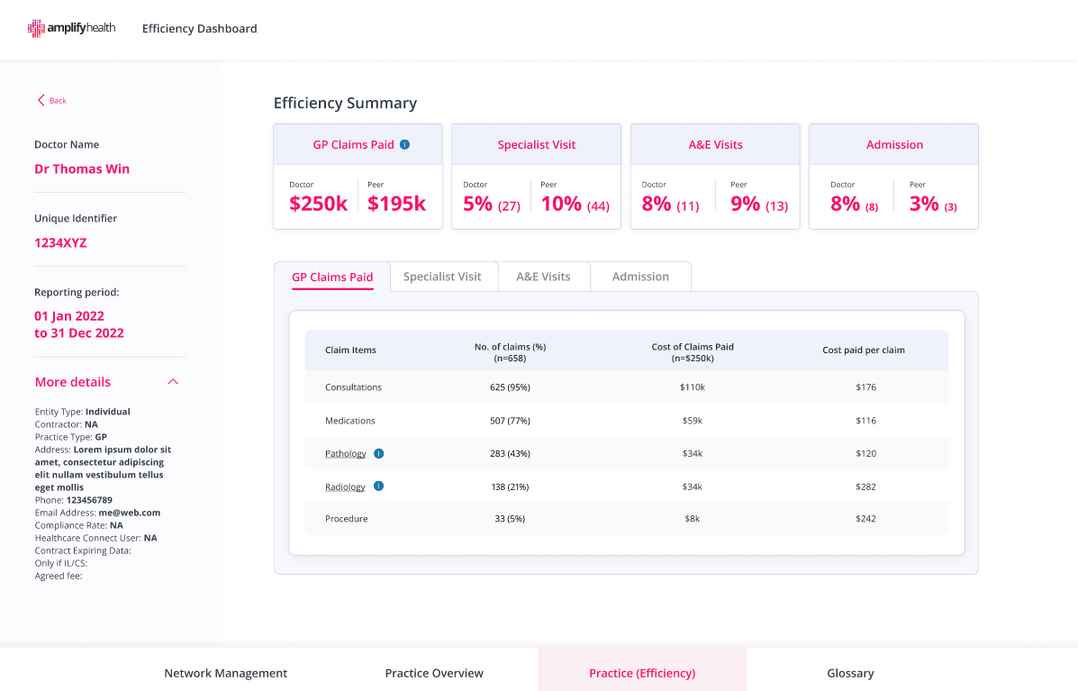
Outpatient Profile Features
Panel Groups
Analyse direct and indirect outpatient panel groups within the network through external panel administrators. Optimise high-value, efficient outpatient networks by prioritising on common performance measures.
Claims Compliance
Monitor compliance of outpatient claims to direct billing agreements and adherence to panel agreed changes.
Rate Differences
Understand and reduce variation between GP and specialist providers’ rate of investigations, referral, and admissions to drive more consistent costs and outcomes.
Individual Practice Profiles
Available for each clinic or practitioner, with overall performance scores based on peer cohort benchmarks.
Patient Metrics
Encourage patient-centric care with patient allocation metrics that differentiate ad-hoc outpatient visits from members who regularly visit specific outpatient providers.
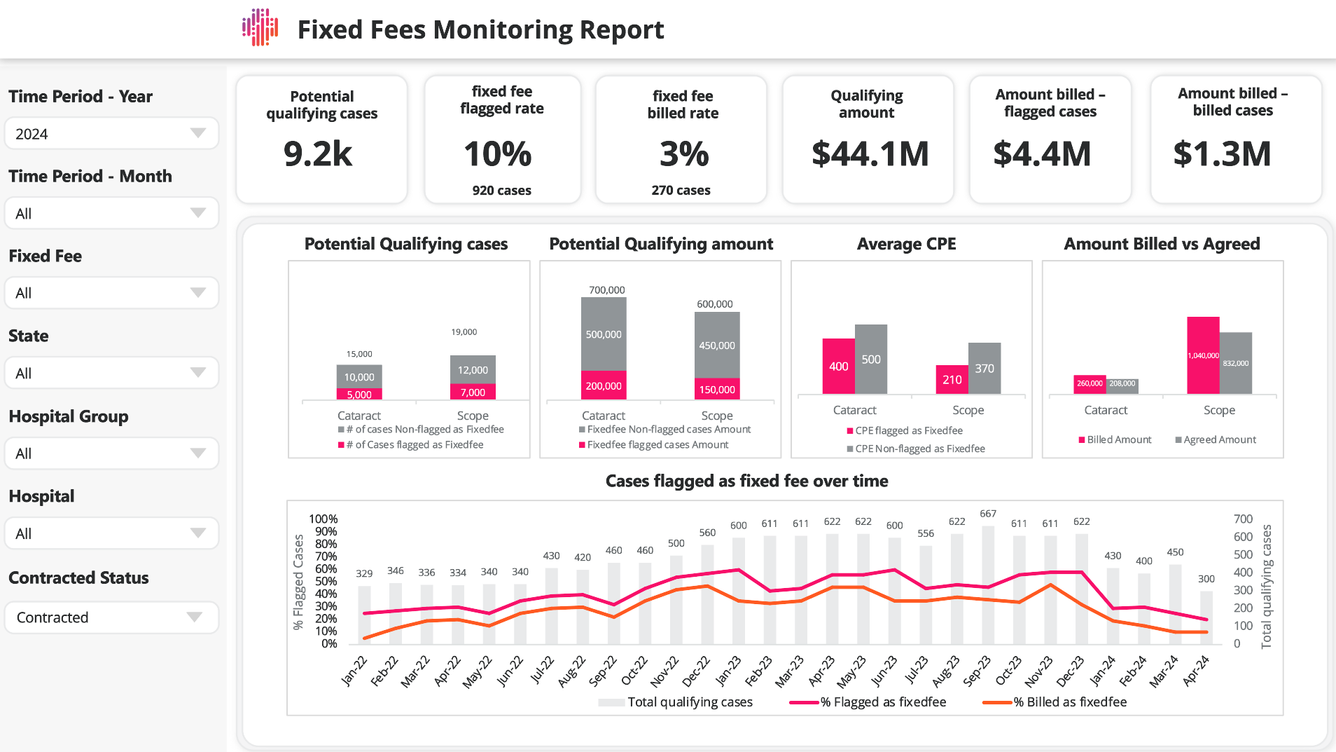
Bundled Pricing, Reference Fees Monitoring
Design fee packages or fixed-fee bundles.
Amplify Health's Bundled Pricing & Fee solution combines clinical advisory and data-led models to benchmark prices and develop new fee proposals.
Reference fee analytics provide statistical insight into claims variation across different cost categories.
Automated tools for Bundled Fee Monitoring encourage increased adoption and quantify savings over time.
Key Features
Adjust for claims outliers and complex conditions to ensure bundled price recommendations account for real-world differences in member and treatment profiles.
Identify potential areas for alternative reimbursements beyond fee for service, such as fixed fee, bundled payments or per-diem arrangements.
Define appropriate contracting terms based on conditions, procedures or medications for robust alternative fee arrangements.
Evaluate cost variations and recommended fee levels within the chosen opportunity scope, either within the same hospital or across comparable institutions.
Initial engagement to assess and design bundled fees or reference prices are offered as an Advisory service supported by client’s data

Engage Our Provider Management Advisory
Our on-site and virtual service over 3 to 6 months provides tailored support to:
- Establish Provider Risk Management approaches and engagement framework
- Identify high-value opportunities and interventions based on measured performance insights
- Equip your teams with the knowledge and confidence to handle provider objections, rebuttals, and questions
- Led by clinical and actuarial experts with over 40 years of collective experience in Provider Risk Management

All representations of outcomes and key results referenced herein are based on previous engagements. Actual product-specific results may vary depending on eligibility criteria for claims processing, pre-existing solutions, and current assessor practices, where applicable. For Clinical Encoder, the actual results may vary based on data quality and variability.